Glaucoma is an eye disorder characterised by raised pressure within the eyeball, resulting in progressive damage to the optic nerve in the eye and irreversible vision loss.
It is known as a silent thief of sight because it often goes undetected until substantial vision loss is already present. Depending on the type of glaucoma, it sometimes manifests as a gradual blurring of the peripheral (and eventually, central) vision. In other types, it may present as sudden blurred vision with severe eye pain and headaches. There is no known cure for glaucoma, although it can be treated with surgery and medication to slow its progression and preserve sight for a patient's lifetime.

Glaucoma is caused by high intraocular pressure resulting in damage to the optic nerve. This pressure builds up when the fluid within the eye, known as the aqueous humour, does not drain properly. Aqueous humour is constantly produced and needs to flow out through a tiny channel near the front of the eye. If the drainage angle is not working properly, pressure builds and can damage the optic nerve.
At Lumin Eye Specialists, our glaucoma doctors offer comprehensive glaucoma evaluations and screenings in Singapore with the goal of detecting the disease before symptoms develop, or before serious vision damage is done.
High Intraocular Pressure (IOP) – An increase in intraocular pressure leads to optic nerve damage and vision loss.
Previous Eye Injuries or Surgery – Some people develop glaucoma after an eye injury or surgery.
Systemic Health Conditions – Some health conditions can increase the risk of developing glaucoma, such as diabetes, high blood pressure, heart disease and sickle cell anaemia.
Age – People over the age of 60 have a higher risk of developing glaucoma. Eye screening for glaucoma is essential for the early detection of the disease.
Family History – Some cases of glaucoma may be hereditary. Having a family history of glaucoma increases the risk of developing the condition.
To diagnose glaucoma, our clinic conducts the following tests:
Glaucoma is a leading cause of blindness if left undiagnosed or untreated. The key to preserving sight
lies in early detection and treatment. This is especially important since glaucoma often progresses
(irreversibly) without any noticeable signs in its early stages.
This is why regular eye exams are crucial, particularly for those at higher risk of developing glaucoma.
Early diagnosis and treatment can effectively manage glaucoma and prevent vision loss.
Depending on the results of your evaluation, your ophthalmologist will advise you on an appropriate course of treatment. This usually involves:
Eye Drops – Prescription glaucoma eye drops can lower eye pressure by improving how fluid drains from the eye.
Oral Medications – Medications may be prescribed alongside or in replacement of eye drops. Common medications for glaucoma include beta-blockers and carbonic anhydrase inhibitors, which can improve drainage or slow the creation of fluid in the eye.
Laser Treatment – Among eligible patients, laser treatments can increase the drainage of aqueous humour from the eye, lowering the eye pressure. These include:
- Laser Trabeculoplasty – This treatment is often recommended for patients who cannot tolerate eye drops or have not responded well to medications. Trabeculoplasty opens up the drainage area to reduce intraocular pressure, preventing vision loss.
- Cyclodiode Laser Treatment – This laser treatment uses a diode to target and treat some of the tissue in the eye that produces aqueous humour. Cyclodiode lowers the production of aqueous humour, helping to reduce intraocular eye pressure.
- Laser Iridotomy – Also known as laser peripheral iridotomy (LPI), this treatment involves making a tiny hole in the iris using a laser to widen the angle in angle-closure glaucoma cases, allowing fluid to drain more easily.
Microsurgery – In more advanced cases of glaucoma that do not respond to other
treatments, surgical intervention may be necessary.
One approach is the minimally invasive glaucoma surgery (MIGS). It involves inserting tiny
devices or implants into the eye to create a new drainage pathway for the aqueous humour. MIGS
reduces intraocular pressure and can be done at the same time as other procedures, such as
cataract surgery. Recovery from MIGS is typically shorter compared to traditional glaucoma
surgeries.
However, while glaucoma surgeries can lower eye pressure to prevent further vision loss, they
cannot improve or restore vision that has already been lost. The damage inflicted on the optic
nerve by glaucoma is considered permanent and irreversible.
We are trained in surgery using minimally invasive glaucoma implants which are proven to be effective and safe. Reach out to our specialist eye clinic for a detailed glaucoma evaluation in Singapore today.
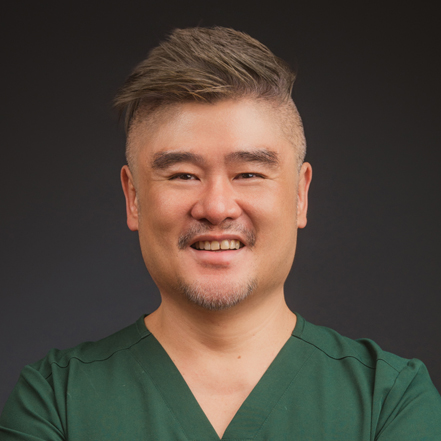
Dr Don Pek
Senior Consultant Ophthalmologist
Dr Don Pek is a Senior Consultant Ophthalmologist with over 15 years of experience in the field, in particular glaucoma surgery and complex cataract surgeries. He completed his general ophthalmology training in Singapore and Edinburgh, UK, followed by a specialised fellowship in Canada focused on Anterior Segment and Cataract Surgery. Dr Pek is dedicated to improving his patients' quality of life through caring for and preserving their vision as far as possible.

Dr Clarissa Cheng
Senior Consultant Ophthalmologist
Dr Clarissa Cheng is a Senior Consultant Ophthalmologist with more than 15 years of experience in the field, in particular glaucoma and retinal disorders. A Gold Medal award winner in the MOH specialist board examinations, Dr Cheng went on to complete her sub-specialty fellowship at the Manchester Royal Eye Hospital in 2018. Besides her clinical practice, Dr Cheng remains involved in the mentoring of future doctors and ophthalmologists through the teaching of medical students.
